Pfizer has announced that the US Food and Drug Administration (FDA) has approved Besponsa (inotuzumab ozogamicin) for the treatment of adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL). Besponsa was reviewed and approved under the FDA’s Breakthrough Therapy designation and Priority Review programs.
“The approval of Besponsa is an important step forward for adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia, a rare disease that can be fatal within a matter of months if left untreated,” said Liz Barrett, global president, Pfizer Oncology. “Besponsa will help address a significant need for new treatment options in B-cell acute lymphoblastic leukemia, and may help more patients reach stem cell transplant, which provides the best chance for long term remission. We’re proud to build on our continued commitment to patients with hematologic malignancies, and will continue our work to find new treatments in acute lymphoblastic leukemia and other blood cancers.”
The approval was based on results from the phase 3 INO-VATE ALL trial, a randomized, open-label, international, multicenter study evaluating the safety and efficacy of Besponsa compared with Investigator’s choice of chemotherapy in 326 adult patients with relapsed or refractory B-cell ALL.
“Based on the results seen in the INO-VATE ALL trial, Besponsa improved multiple efficacy measures, including rates of hematologic remission, MRD-negativity and stem cell transplantation,” said Hagop M. Kantarjian, M. D., INO-VATE ALL lead study investigator and professor, The University of Texas MD Anderson Cancer Center. “I look forward to seeing the impact this important new therapy may have on my patients.”
The complete remission rate (CR/CRi) for patients treated with Besponsa was 81 per cent [95% CI: 72%-88%] compared to 29 per cent with chemotherapy [95% CI: 21%-39%]. Among patients achieving CR/CRi, those treated with Besponsa also demonstrated a higher rate of minimal residual disease (MRD) negativity (78% [95% CI: 68%-87%]) compared to those treated with chemotherapy (28% [95% CI: 14%-47%]). Forty-eight percent of patients treated with Besponsa proceeded to hematopoietic stem cell transplantation (HSCT) compared to 22 per cent treated with chemotherapy. The median overall survival (OS) for patients treated with Besponsa was 7.7 months [95% CI: 6.0, 9.2] and 6.2 months [95% CI: 4.7, 8.3] for patients treated with chemotherapy. The analysis of OS for patients treated with Besponsa compared to chemotherapy did not meet the pre-specified boundary for statistical significance (HR: 0.75 [97.5% CI: 0.57-0.99]).
The US labeling for Besponsa includes a boxed warning for hepatotoxicity, including hepatic veno-occlusive disease (VOD), also known as sinusoidal obstruction syndrome (SOS), and increased risk of post-HSCT non-relapse mortality. Veno-occlusive disease, including fatal and life-threating VOD, occurred in 14 percent of patients treated with Besponsa. A higher post-HSCT non-relapse mortality rate occurred in patients treated with Besponsa (39%) than chemotherapy (23%).1 In patients treated with Besponsa, the most common (=20%) adverse reactions were thrombocytopenia, neutropenia, infection, anemia, leukopenia, fatigue, hemorrhage, pyrexia, nausea, headache, febrile neutropenia, transaminases increased, abdominal pain, gamma-glutamyltransferase increased, and hyperbilirubinemia.
Pfizer is committed to helping patients gain access to Pfizer medicines, including Besponsa, and related educational tools, resources and services, regardless of their financial or health insurance status through the company’s patient assistance programmes.
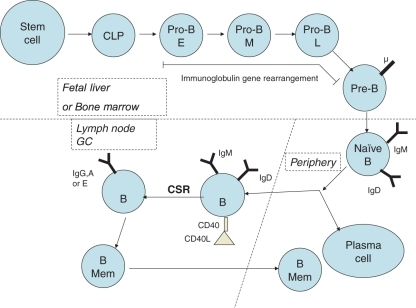
Besponsa is an antibody-drug conjugate (ADC) composed of a monoclonal antibody (mAb) targeting CD22, a cell surface antigen expressed on cancer cells in almost all B-ALL patients, linked to a cytotoxic agent. When Besponsa binds to the CD22 antigen on B-cells, it is internalized into the cell, where the cytotoxic agent calicheamicin is released causing cell death. Besponsa is administered as a one-hour intravenous infusion that can be given in the outpatient setting of care for appropriate patients.
Besponsa originates from a collaboration between Pfizer and Celltech, now UCB. Under the terms of this agreement, Pfizer has sole responsibility for all commercialization, manufacturing and clinical development activities for this molecule. Pfizer also collaborated with SFJ Pharmaceuticals Group on the registrational programme (INO-VATE ALL) for Besponsa.
Us fda approves pfizer's besponsa, treat adults with relapsed, refractory b-cell precursor all